Your gut is your second brain
Research suggests that people living with Crohn’s or Colitis may be twice as likely to experience Mental Health problems as the general population.
There is a relationship between Crohn’s & Colitis and mental health – it’s called the Brain-Gut axis.
The term Brain-Gut axis refers to this direct link between mental and physical health in conditions such as Crohn’s and Colitis. Anxiety or depression can lead to new gut symptoms. Equally, experiencing symptoms in your gut has been linked to developing new psychological symptoms. The inflammation in your gut which causes some of the symptoms of Crohn’s or Colitis can also directly affect how you feel.
The good thing is that keeping gut inflammation under control may directly help to improve your mental health. This makes it even more important to keep looking after yourself and find a treatment that works for you. Early evidence also suggests that some medicines used to treat mental health problems such as antidepressants may have a positive effect on improving gut inflammation.
Did you know?
Your gut microbiome (the microbes living in your gut) plays a vital role in supporting your mood. Up to 95% of serotonin (one of the ‘happy chemicals’) is produced in your gut!
When you get those butterflies in the pit of your stomach, that’s the gut-brain connection. When you feel hungry, that’s the same connection and when you feel anxious, that’s the gut-brain connection too!
Info from Guts UK
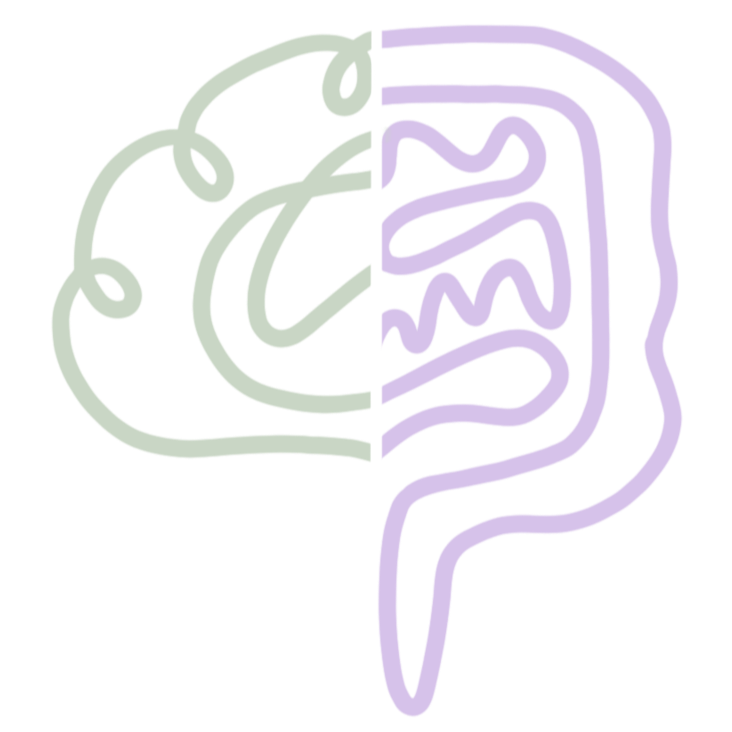
Brain-Gut Connection
The brain-gut connection describes the two-way communication between the central nervous system (brain and spinal cord) and the enteric nervous system (the network of neurons lining the gastrointestinal tract). This bidirectional pathway influences digestion, mood, immune function, and overall well-being.
Key components
Vagus nerve: The primary neural highway linking brain and gut, carrying signals that regulate gut motility, secretion, and inflammation.
Enteric nervous system (ENS): Often called the “second brain,” the ENS contains millions of neurons that control digestion independently but also interact with the central nervous system.
Gut microbiota: Trillions of bacteria and other microbes in the gut produce metabolites (like short-chain fatty acids), neurotransmitters (such as serotonin), and immune-modulating compounds that affect brain function.
Immune system and inflammation: Gut barrier integrity and immune signaling can influence systemic inflammation, which in turn impacts brain health and mood.
How it affects health
Mood and mental health: Many neurotransmitters involved in mood regulation are produced or regulated in the gut. Disruptions in gut microbiota or chronic gut inflammation are associated with anxiety and depression.
Digestive disorders: Conditions like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and functional dyspepsia often involve altered brain-gut signaling, which can amplify pain and bowel symptoms.
Stress response: Psychological stress affects gut motility, secretion, and permeability; conversely, gut disturbances can heighten stress sensitivity and cognitive symptoms.
Sleep and cognition: Gut microbiota and inflammatory signals can influence sleep quality, cognitive function, and fatigue.
Practical ways to support a healthy brain-gut axis
Balanced diet: Emphasize fibre-rich plants, whole grains, fermented foods (yogurt, kefir, sauerkraut), and varied plant foods to support diverse gut microbiota.
Manage stress: Techniques like mindfulness, deep breathing, progressive muscle relaxation, and gentle movement help regulate nervous system activity and gut function.
Regular sleep schedule: Consistent sleep supports microbiota rhythms and reduces inflammation.
Physical activity: Moderate exercise promotes gut motility, microbial diversity, and mood.
Avoid unnecessary antibiotics and limit excessive alcohol: Both can disrupt microbiota balance.
Probiotics and prebiotics: Certain probiotic strains and prebiotic fibers may help for specific conditions; discuss options with a healthcare provider.
Work with professionals: For persistent gut or mood symptoms, consult a gastroenterologist, mental health professional, or dietitian familiar with the brain-gut axis.
When to seek help
Persistent changes in bowel habits, unexplained weight loss, severe abdominal pain, blood in stool, or prolonged low mood, anxiety, or cognitive decline warrant medical evaluation.
Quick takeaway The brain and gut communicate continuously through neural, immune, hormonal, and microbial pathways. Supporting gut health through diet, sleep, stress management, and lifestyle can positively influence mood and overall well-being. If symptoms are severe or persistent, seek professional care.